Seeing is believing with new eye surgery
When Cecilia Apiedu got a call from her ophthalmologist at UI Health, offering her the chance to be the first patient in Chicago to try a new treatment for an eye condition that was threatening her vision, she “was dancing up and down.”
“I realized I was really having trouble with my vision two years ago when I went back to school and needed to do a lot of reading,” said Apiedu, now a certified nursing assistant.
Then, about a year ago, the Glenwood woman’s vision began to decline dramatically. She saw halos and after-images that persisted when she closed her eyes, progressing to double-vision.
“I was always experimenting to find a way to manage,” she said, like perching the TV on her lap when she watched.
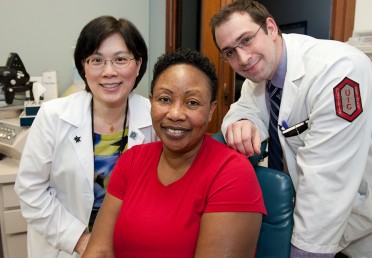
Cecilia Apiedu, center, soon after surgery, with ophthalmologists Jennifer Lim and Senad Osmanovic. Photo: Roberta Dupuis-Devlin/UIC Photo Services
Apiedu had vitreomacular adhesion, or VMA. With this condition, the vitreous — the clear jelly-like substance filling the center of the eye — shrinks with age and pulls the retina inward. Vision becomes distorted, and if the retina tears, serious vision loss or blindness can result.
UI Health is the first center in Chicago to offer a new, nonsurgical treatment for the disease, which affects half a million people in the U.S.
“Ms. Apiedu is in many ways a typical VMA patient,” said Jennifer Lim, director of retina services and the physician who treated Apiedu.
VMA is most common in women over 50, said Lim, who holds the Marion H. Schenk Esq. chair in ophthalmology for research of the aging eye in the College of Medicine.
In Apiedu’s case, Lim could see a hole developing, an indication that she would need surgery.
The surgery — which Lim has done successfully many times — is difficult for the patient. The ophthalmologist removes the vitreous from the center of the eye, peeling it away from the retina, then inserts a bubble into the eye to help the macular hole heal.
After surgery, the patient must lie face down for two weeks.
Instead, Apiedu sat comfortably in an exam room in the UI Health retina clinic Feb. 13 and received an injection in her left eye of ocriplasmin, a drug just approved by the FDA in November and marketed in the U.S. as Jetrea.
The procedure took less than 10 minutes. An hour later, photos of her eye showed improvement.
Jetrea, an enzyme, quickly dissolves the natural glue that fastens the vitreous to the retina.
The treatment is a major advance because VMA patients can avoid surgery, said Rohit Varma, professor and chair of ophthalmology and visual sciences.
Varma, an expert on quality-of-life assessment in eye disorders and treatment, testified at the drug’s FDA approval hearing.
Apiedu said that, except for a brief feeling of pressure, the injection was painless.
For the first few minutes after the injection, she saw a “kaleidoscope” view of the world, but 24 hours after surgery, her vision was significantly improved.
Lim said imaging studies of the eye showed the vitreous was no longer pulling on the macula.
Apiedu was enthusiastic.
“I want for other people to benefit from this,” she said.
