‘Decoy’ protein works against multiple SARS-CoV-2 variants
A drug treatment that acts as a decoy against SARS-CoV-2 was highly effective at preventing death and lung damage in humanized animal models of severe COVID-19 disease, according to a Nature Chemical Biology study from researchers at the University of Illinois Chicago. The study suggests that the drug has the potential to treat COVID-19 patients, including those who are infected with aggressive SARS-CoV-2 variants.
The study’s senior lead author is Asrar Malik, professor in the department of pharmacology and regenerative medicine at the UIC College of Medicine. Jalees Rehman, professor in the department of pharmacology and regenerative medicine and the department of medicine, is a co-lead author of the study, “Engineered ACE2 decoy mitigates lung injury and death induced by SARS-CoV-2 variants.”
“While vaccines remain the best option for preventing infections, long-term complications and death from COVID-19, there is an urgent need for the development of effective treatments for vulnerable patients, especially as new variants continue to arise,” Rehman said.
“Vulnerable individuals who are at risk of developing severe COVID-19 include those who are unvaccinated or immunocompromised and therefore their immune system cannot protect them as well even after receiving vaccinations and boosters,” he said. “In addition, new variants of SARS-CoV-2, such as the most recent omicron variant, may partially evade the immune system and can cause breakthrough infections. For all the vulnerable patients, we need to create an array of treatments so that health care providers can choose the most appropriate drug or combination of drugs, depending on the individual patient’s disease stage and severity.”
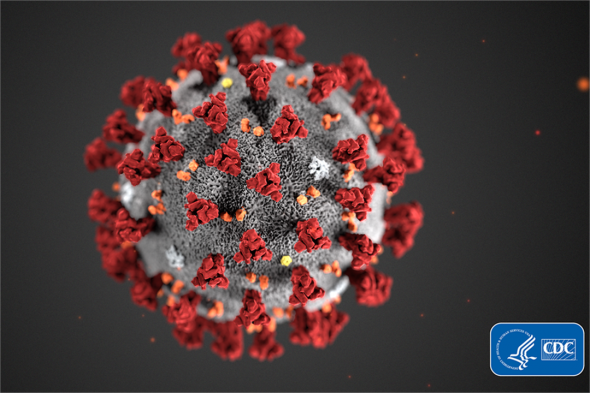
The drug treatment, developed through a partnership between UIC and the University of Illinois Urbana-Champaign, consists of an artificially engineered ACE2 protein designed with unprecedently high binding capacity for the spike protein of SARS-CoV-2, which binds to natural ACE2 protein receptors located on human cells and causes COVID-19. The drug works by competing for the spike protein and soaking up viruses before they can bind and enter cells.
In animal studies of severe COVID-19, the researchers used mouse models designed to carry the human ACE2 protein. With multiple treatment regimens, infected mice were given the drug intravenously. The researchers found that mice receiving the treatment showed markedly reduced death and no significant evidence of severe acute respiratory syndrome, the hallmark of the disease and primary cause of death. The mice receiving the drug also regained appetite and weight, which are signs of recovery.
The benefits were seen even when mice were exposed to the aggressive gamma variant, suggesting the drug’s broad applicability against newly emerging COVID-19 variants.
“The reduced rates of fluid buildup in the lungs and of death in treatment group illustrates the potential of the ACE2 decoy to help people with severe COVID-19,” Malik said. Severe fluid buildup in the lung is one of the complications of COVID-19 that makes it difficult for patients to breathe and leads to the need for a ventilator.
In additional studies, the researchers tested how well the decoy would bind and neutralize multiple variants of SARS-CoV-2. They observed that the decoy was able to bind to the spike proteins from all the variants tested, which included the alpha, beta, gamma, delta and epsilon variants, which were available at the time of the study. They also found that it bound equally, if not better, to the variants than it did to the original strain of the virus.
“Considering the emergence of omicron, it is very good news that the ACE2 decoy was able to bind and neutralize several variants, and this reinforces the potential of this drug as a treatment, including against new or future variants of the virus,” Rehman said.
One of the exciting things about the drug, Rehman said, is that it has the potential to be used in combination with other drugs, especially those that prevent replication of the virus that has already entered cells or drugs that prevent an excessive immune response, which itself can worsen COVID-19 complications.
The researchers also found that the decoy protein could be delivered by inhalation directly to the lungs of mice.
Even though many of the treated animals recovered, a few mice developed lung scarring over time. According to the researchers, this highlights the importance of also studying and developing therapies for long-term COVID-19 complications, such as long COVID.
The research was funded in part by grants from the National Institutes of Health (P01HL060678, P01HL151327, R01HL154538, R01HL152515. R43AI162329, R01HL157489, T32HL007829).
UIC’s Lianghui Zhang, assistant professor in the department of pharmacology and regenerative medicine, and UIUC’s Erik Procko, associate professor in the department of biochemistry, are also co-lead authors of the study.
Additional co-authors of the paper are Shiqin Xiong, Matthew Lindeblad, Laura Cooper, Lijun Rong, Anthony Gugliuzza, Soumajit Dutta, Matthew Chan, Timothy Fan, Keith Bailey, Diwakar Shukla and Kui Chan.


