Sensing infection, suppressing regeneration
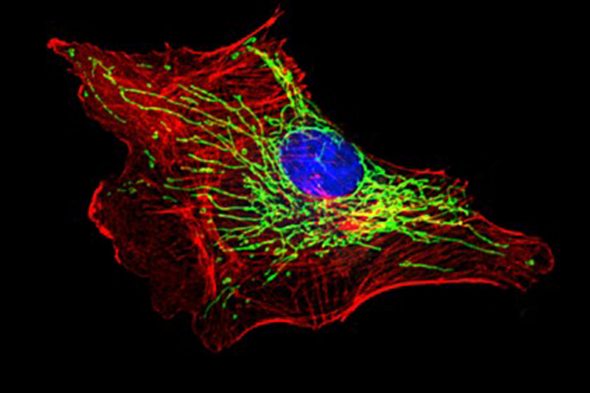
In a new peer-reviewed publication, University of Illinois at Chicago researchers describe how the body’s response to inflammation, which helps to fight many kinds of infections, also can counterproductively suppress much-needed cell repair and regeneration in blood vessels.
In the study, which is published in Immunity, the researchers describe an enzyme that blocks the ability of blood vessel cells to self-heal. By studying mice with sepsis — a condition caused when the body’s inflammatory response to a bloodstream bacterial infection spirals out of control — they found that removal of the enzyme allows cells to fully regenerate.
“When cells are faced with an injury or an infection, it seems that they make a ‘fight’ or ‘fix’ choice,” said UIC’s Asrar Malik, senior author of the study and the Schweppe Family Distinguished Professor and head of pharmacology at the College of Medicine. “Inflammation is the ‘fight’ response, and the cells appear to delay regeneration while amplifying the inflammatory response.”
“We think that over time cells have evolved to favor fighting an infection over repairing damaged cells, but in some cases, this preference to fight puts the body at further risk,” said Dr. Jalees Rehman, co-senior author and UIC professor of medicine, pharmacology and bioengineering at the College of Medicine. “Especially when the immune response of the body to an infection is so excessive that it damages vital organs such as the lungs, it is absolutely vital that we learn how to help cells restore their ability to regenerate and resolve the inflammation.”
Rehman said that the enzyme — named cGAS — acts as a DNA sensor that is being activated by the DNA released by damaged mitochondria of the blood vessel cells.
“We showed that when the sensor is removed, blood vessel endothelial cells shift their balance towards restoration and regeneration,” Rehman said.
In an experimental model of bacterial sepsis, mice lacking this DNA sensor had much higher rates of survival and showed rapid regeneration of the blood vessels in the lung.
“It’s possible that the degree to which this DNA injury sensor gets activated contributes to why some individuals survive a severe condition like sepsis,” he said. “Suppression of regeneration is especially concerning in the elderly. Our study suggests that further study of this DNA sensor might provide provocative new areas for research to improve endogenous regeneration.”
Co-authors on the paper are UIC’s Long Shuang Huang, Zhigang Hong, Wei Wu, Shiquin Xiong, Ming Zhong and Xiaopei Gao.
The study was funded by grants from the National Institutes of Health (R01HL45638, P01HL60678, T32GL007829, R01HL118068 and R01HL90152).
Categories
Health Sciences Colleges, Research
Topics
College of Medicine, inflammation, pharmacology, regenerative medicine, tissue regeneration
