Study shows protective role sex steroids play in COVID-19
A new paper from a UIC researcher shows evidence that suggests sex steroids may play a role in protecting against COVID-19 symptoms.
“Sex and Covid-19: A protective role for reproductive steroids,” by Graziano Pinna, research associate professor in psychiatry, analyzes existing research to look at reasons why COVID-19 symptom severity and mortality are more frequent in men than in women and in older people. His paper suggests female reproductive steroids play a protective role.
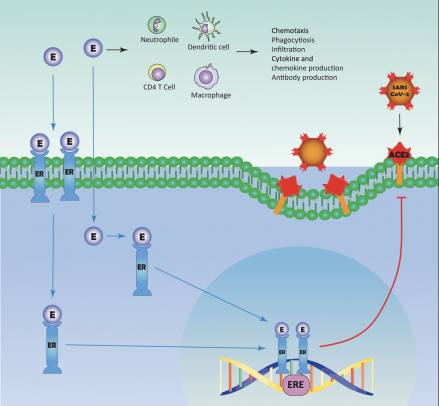
Female reproductive steroids, estrogen and progesterone and its physiologically active metabolite, allopregnanolone, provide anti-inflammatory functions, reshape competence of immune cells, stimulate antibody production and promote respiratory epithelial cell repair, and inhibit the ACE2 receptor, the door of access for the novel coronavirus (SARS-CoV-2) to infect the organism, suggesting they may protect against COVID-19 symptoms, according to Pinna’s report. The paper is published in Trends in Endocrinology and Metabolism.
Pinna became interested in the role of reproductive steroids in COVID-19 pathology in March when early case reports showed COVID-19 positive pregnant women who had no COVID-19 symptoms, had escalated symptoms — severe enough to require intensive care — immediately after giving birth. The severity of symptoms coincided with a rapid drop of estradiol, progesterone, and allopregnanolone.
“Hormones that help sustain the pregnancy – like progesterone — are 100 times more concentrated in a pregnancy’s third trimester. Estradiol, allopregnanolone, and progesterone all have important anti-inflammatory functions and are involved in resetting the immune system. This suggests that pregnant women became symptomatic, and some were even admitted to the ICU, after delivering their babies because of the rapid drop in these hormones,” said Pinna. “The correlation was really striking.”
According to recent CDC data, in the United States, 38,071 women who were pregnant contracted COVID-19, with 51 deaths — 0.13%. For non-pregnant women, the death toll is 2%.
“Pregnant women are 15 times less likely to die from COVID than other women,” said Pinna.
There is a difference between the severity of symptoms, and intensive care hospitalization between men and women with COVID-19, with women being more resistant. It was thought that female hormones protected women, but it was difficult to ascertain why, said Pinna.
“This observation in pregnant women provides significant scientific background, not only as to why women are more protected than men, but also why older people are less protected than younger people because we know the older you are, the more decreased your hormones are,” said Pinna.
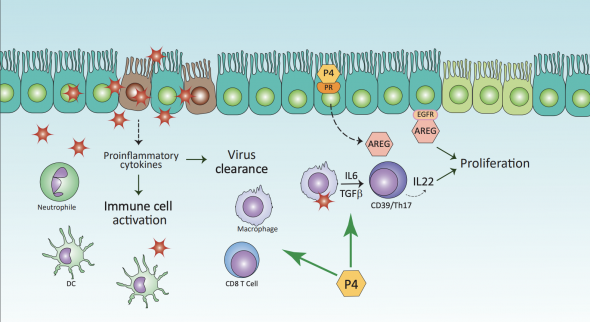
Pinna’s paper also discusses the importance of reproductive hormones in stimulating the production of antibodies and promoting lung cell repair after virus infection and fighting against the ‘cytokine storm’ — an immune response where the body starts to attack its own cells and tissues rather than just fighting off the virus.
“Progesterone and allopregnanolone can block the incredible overreaction of the inflammatory system, repressing it and avoiding the over-expression of pro-inflammatory cytokines,” said Pinna.
Reproductive hormone protection from COVID symptoms may be warranted by oral combinations of hormonal contraceptives or by treatment with hormone replacement therapy against hypoestrogenism in postmenopausal women. Pinna said clinical trials to evaluate the efficacy of progesterone or estradiol to improve COVID-19 symptoms in men and post-menopausal women are underway.
Additionally, nutrition may also play a role when diets are enriched with phytoestrogens – plant-produced ‘estrogen’ — (in foods such as soybeans, lentils, oats). Phytoestrogens have the ability to bind directly to human estrogen receptors, or can be converted to estradiol by the microbiome. The microbiome is the collective genomes of the microbes (composed of bacteria, bacteriophage, fungi, protozoa, and viruses) that live in the gut.
“Nutrition is very important and there hasn’t been much talk about it,” Pinna said. “It is important because it is something we can take care of each day to boost the immune system and make our bodies stronger against COVID.”
