New research identifies key target in relationship between white blood cells, inflammation
Inflammation is the alarm system of the body; effective in signaling emergencies, but hazardous if triggered too often. A new research paper from scientists in the University of Illinois Chicago Department of Pharmacology and Regenerative Medicine reveals a potential new drug target to control autoimmune and chronic inflammation diseases such as atherosclerosis and metabolic syndrome.
The paper, which identifies a key trigger in the white blood cell response to cellular injury and disease, was published in the journal eLife. The research was led by Shweppe Family Distinguished Professor Asrar Malik and Research Assistant Professor Dr. Anke Di, a member of Malik’s research group and an expert in ion channel regulation of macrophage plasticity.
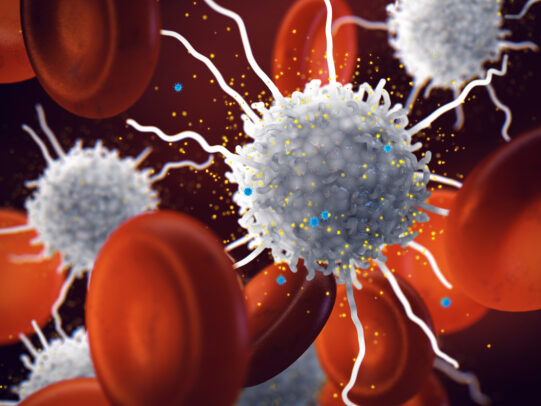
Inflammation occurs when cells detect nearby damage or infection, triggering a complex sequence of cellular events. In the white blood cells called macrophages, which surround and consume foreign pathogens, activation of the NLRP3 inflammasome complex initiates their attack. But this process must be carefully controlled so as not to produce excessive inflammation, the cause of many chronic diseases and dangerous acute symptoms in illnesses such as COVID-19.
In the new paper, researchers from UIC, the University of Chicago and Shanghai Jiao Tong University filled in the sequence of events that lead to NLRP3 activation. Previously, the team zeroed in on an ion channel called TWIK2, the activity of which initiates the formation of NLRP3. But what signal flips this switch for inflammation?
The new paper pinpoints a protein called rab11a, which is sensitive to elevated levels of calcium inside the cell — an indicator of nearby tissue damage. Once turned on, rab11a causes TWIK2 to move from internal storage to the cell surface, where its activity triggers the NLRP3 inflammasome.
By fleshing out this assembly line of proteins, the researchers mark its components as potential targets for new drug treatments. Blocking rab11 activity could prevent or reduce inflammation and avoid its damaging effects in acute or chronic disease. Di and Malik have multiple grants to continue this work, and the group is currently collaborating with Yamuna Krishnan, a chemical biologist at the University of Chicago, to develop an anti-inflammatory drug based on the findings.
This research was supported by grants from the National Institutes of Health. In addition to Krishnan, Di and Malik, co-authors on the paper include Mohammad Anas, Jingsong Xu, Bisheng Zhou and Peter Toth of UIC, and Long Shuang Huang of Shanghai Jiao Tong University.