Two-pathway approach enables better anti-platelet drug for after heart attack, stroke
Platelets are blood cells that patch up wounds and stop bleeding inside and outside the body. But when platelets overreact, they also can clog blood vessels and potentially cause heart attack and stroke. Even after treatment for a stroke or heart attack, platelet activity can exacerbate damage — they rush into the organ injured by the lack of oxygen to block small blood vessels in the tissue and release harmful factors.
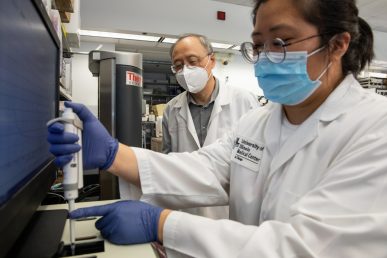
For more than a decade, the University of Illinois Chicago laboratory of Dr. Xiaoping Du has been working on a new drug to prevent this secondary effect, called an ischemic reperfusion injury. A new discovery, described in a Nature Communications paper, brings their goal of a selective platelet inhibitor closer to reality thanks to a new understanding of how two important cellular pathways crossover.
The authors created a single peptide that blocks both pathways at once, preventing the platelets from releasing factors that can cause inflammation, blockage or thrombosis of small blood vessels. However, the drug does not affect the ability of platelets to stick to wounds and to each other, maintaining their primary role in sealing up the blood vessels.
“Inflammation and clotting usually go hand in hand, and classic antiplatelet drugs poorly affect inflammation but cause bleeding,” said Du, professor of pharmacology and regenerative medicine in the College of Medicine. “Ours is a new drug that can greatly inhibit both thrombosis and inflammation without causing bleeding. There’s no really good way to do this at the moment, so this is revolutionary.”
Du’s group made previous progress toward developing this drug by focusing on a cellular receptor called integrin. Integrins help platelets stick to the site of a wound as well as to each other, forming a barrier that stops bleeding.
But after this attachment, integrin also causes platelets to release factors that cause additional damage and complications after a heart attack or stroke. Previous antiplatelet drugs were unsuccessful at preventing secondary damage after heart attacks or strokes.
The reason why turned out to be a second trigger for granule secretion, mediated by a G-protein coupled receptor. In the new paper, Du and colleagues found that integrins directly bind and “crosstalk” to G protein pathways. When integrin is blocked, this second pathway is enhanced, causing continued granule secretion.
Du and colleagues identified and developed a peptide that can inhibit the activity of both integrin and G protein pathways of granule secretion. The team found that the drug worked in both cellular and animal models, preserving the primary clotting abilities of platelets but negating their unintended damage.
If confirmed in clinical trials, Du said the drug could be useful for treating patients after heart attack or stroke, protecting them from ischemic reperfusion injury. He is working with the UIC Office of Technology Management on bringing the treatment to market.
In addition to Du, co-authors on the paper include Yaping Zhang, Xiaojuan Zhao, Bo Shen, Yanyan Bai, Claire Chang, Aleksandra Stojanovic, Can Wang, Andrew Mack, Gary Deng, Randal Skidgel and Ni Cheng.