$2.2 million federal grant funds study of diabetes drug in wound healing
A drug taken orally to control blood-sugar levels in diabetic patients may promote wound healing when applied directly to injured tissue, according to a researcher at the UIC College of Applied Health Sciences.
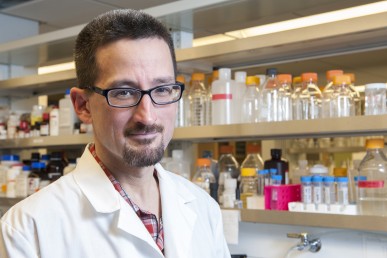
Timothy Koh, professor of kinesiology and nutrition, UIC College of Applied Health Sciences, is researching wound healing in diabetic individuals.
Timothy Koh, professor of kinesiology and nutrition, will use a four-year, $2.2 million grant from the National Institutes of Health for a translational study of the diabetes drug glyburide for wound healing in humans, beginning this summer. He has been studying glyburide in mice.
Koh says that studies in his laboratory showed that glyburide applied directly to wounds in diabetic mice improved healing. The drug, he says, may modify the activity of macrophages — cells that are crucial in healing.
Research in other laboratories has shown that glyburide inhibits a cellular structure called the NLRP3 inflammasome, “which is kind of a danger-sensor for the immune system,” Koh said.
Other groups, he said, have found that the elevated sugar levels in diabetes may activate the inflammasome.
“When this pathway is activated, an inflammatory response is mounted, macrophages get angry and cause tissue damage,” Koh said.
Sustained activity of the inflammasome may cause chronic inflammation and impaired healing, resulting in chronic wounds, commonly appearing as foot ulcers in diabetic patients.
The human study will enroll 60 older diabetic patients. Half will have their wounds treated with glyburide, and the other half will be treated with a placebo for one month.
Koh suspects that wounded tissue communicates with the bone marrow, where macrophages are produced — and in diabetic patients, the signals may be amplified or extended in duration. He hopes to see whether those signals can be controlled by applying glyburide to the wound.
“We’ll measure inflammatory cells in the wounds, the blood, and the bone marrow,” he said. “We’ve been studying how this treatment works in diabetic mice, and now we will extend these studies to diabetic patients.”
Koh’s current work builds on previous research targeting inflammation in wounds so that healing can progress. He also studies the use of low-intensity vibrations to spur the formation of tissue to heal wounds. Both projects are in collaboration with Dr. William Ennis, clinical professor of surgery and director of UIC’s Wound Healing and Tissue Repair Clinic.
